Judy Ranka is a Lecturer in the School of Occupational Therapy, The University of Sydney
PURPOSE
This aim of this paper is to present an example of how the Occupational Performance Model (Australia) (Chapparo & Ranka, 1996) can be used to guide occupational therapists in their prescription of upper limb orthotics with clients whose hand function has been compromised by spinal cord injury. The example presented is an extension of an action research project originally completed by Ranka, Colyer, Dickson and Chow (1994) in which an earlier version of Occupational Performance (Chapparo & Ranka, 1992) was used as the foundation for an upper limb orthotic program.
BACKGROUND:
Occupational therapists and orthotists have long used upper limb orthotic systems with clients who have wrist and hand weakness or paralysis resulting from spinal cord injury (Anderson, 1965; Lohman, 1982; Mallick, 1965; Cuilford & Perry, 1975; Wilson, McKenzie & Barber, 1974). Reasons include:
| 1 | to prevent deformity through ‘static’ positioning (Chapparo, 1980; Guilford & Perry, 1975; Mallick, & Meyer, 1978). |
| 2 | to promote functional use of the hand through ‘dynamic’ orthoses such as Ranch los Amigos wrist-driven flexor hinge orthoses, the RIC tenodesis splint or various shoulder-driven and myoelectric devices (Chapparo, 1980; Hill & Presperin, 1986; Guilford & Perry, 1975; Nichols, Peach, Haworth & Ennis (1978). |
Orthotics fabricated by occupational therapists are usually viewed as temporary devices (Hill & Presperin, 1986) and constructed of low temperature thermoplastics. Those fabricated by orthotists tend to be constructed of more rigid products such as polypropylene, laminated plastic or metal. Plaster of paris bandage may also be used in situations where resources are limited (Ranka & Zhuo, 1987). Although orthotists specialise in the design and fabrication of orthotics, occupational therapists are often solely responsible for the prescription and fabrication of ‘hand splints’. Even when an orthotist is available, occupational therapists may still identify the need for intervention and provide follow-up orthotic use training.
Considerable evidence exists which supports the need for early and long-term orthotic intervention in clients with upper limb problems resulting from spinal cord injury. For example, Yarkony, Bass, Keenan and Meyer (1985) and others describe biochemical and pathological factors associated with contracture formation and note the speed with which deformity develops (Akeson, Amiel, Abel, Garfin & Woo, 1987; Booth, 1987 Botte, Nickel & Akeson, 1988; Enneking & Horowitz, 1972). Others such as, Brand (1985), Wynn Parry and Berkely (1975) and Guilford and Perry (1975) report the effects of an unsupported joint on secondary deformity elsewhere, for example, when an unsupported wrist rests in flexion and results in secondary extension contractures at the metacarpal-phalangeal joints. Deforming forces created by muscle imbalance have also been described (Perry, 1975); for example, when denervation to the triceps results in a lack of an opposing force to elbow flexion/supination and a wrist extension contracture ensues.
Literature which specifically addresses the use of upper limb orthotics as a method of intervention in this area of practice consists of:
| 1 | descriptions of new orthotic designs and clinical observations of their effect (see for example, Lightbody, 1994; Sutton, 1993, Yarkony, 1990) |
| 2 | guidelines, protocols and instructions for fabrication of orthoses (see for example: Chapparo, 1980; Hill & Presperin, 1986; Mallick & Meyer, 1978; Newsom, Keenan, Maytree & Aguilar, 1969; Wilson, McKenzie, Barber & Watson, 1984; Sargent & Braun, 1986). |
| 3 | surveys of client groups about long-term orthotic use (see for example, Lee, 1988; Martin, 1987; Shepherd & Ruzicka, 1991; Wise, Wharton & Robinson, 1986) |
| 4 | empirical studies of orthotic effect (DiPasquale-Lehnerz, 1994). |
Objective findings reported in the literature indicate that many clients discontinue upper limb orthotic use after they return home (Lee, 1988; Martin, 1987; Shepherd & Ruzicka, 1991), and that factors associated with continued use following return home include, 1) early prescription and use of the orthosis, and 2) client recognition of a functional need for an orthosis. These findings are not surprising when one considers literature associated with the impact of spinal cord injury on psychological functioning and comprehension of information (Partridge, 1994; Patterson, 1993). Others also note the importance of effective teaching and learning strategies on clients abilities to understand information about proposed interventions (Boss, 1994).
Results from empirical studies are limited. DiPasquale-Lehnerz (1994) used an experimental design to investigate the effect of night wear of wrist-hand or hand orthoses of the opponens design on improvements in hand function, range of motion and tenodesis prehension in persons with C6 spinal cord injury. She found no significant differences in this study but acknowledges that client engagement in wheelchair propulsion tasks during the day may have compromised any orthotic effect produced during night wear (DiPasquale-Lehnertz, 1994, p.141). No other empirical studies of orthotic effect have been located in the literature.
Also lacking in the literature are discussions of occupational therapy theoretical bases for the prescription of upper limb orthoses with this population, or studies which go beyond the broad aims of deformity management and improving hand function. Consequently, occupational therapists have little guidance in developing rationales for clinical decisions in this area of practice and controversy remains evident (DiPasquale-Lehnertz, 1994; Spinal Practitioners Group – Sydney, personal communication, October, 1994).
Questions asked include:
| Is orthotic intervention implicated for specific clients or not? Why? |
| How should an orthosis position the wrist and/or hand? |
| What wearing schedule should be adhered to? |
| Over what duration is orthotic intervention required? |
DEVELOPING A GUIDE FOR SERVICE DELIVERY
The Occupational Performance Model (Chapparo & Ranka, 1992, 1996) has been used by occupational therapists as a guide for practice in this area (Ranka, Colyer, Dickson & Chow, 1994). This occurred through action research (Kemmis & McTaggart, 1988) involving the author and occupational therapists working at the Royal Rehabilitation Centre Sydney. Ranka, Colyer, Dickson and Chow (1994) identified that one thematic concern of occupational therapists working in the Moorong Spinal Unit of the Centre revolved around,
| Developing a cohesive approach to orthotic intervention which is theoretically sound, reflects occupational therapy practice and the philosophy of the Occupational Therapy Service in the Centre and gives guidance to current and newly employed therapists. |
Kemmis and McTaggart (1988, p. 12) note that in action research any action taken is deliberate, controlled and critically informed. Action is a careful and thoughtful variation of practice (Kemmis & McTaggart, 1988, p.11). In this project this involved extensive and ongoing values clarification about orthotic intervention, the impact of spinal cord injury on clients lives and occupational therapy practice in this area as reported in the literature. Philosophical discussions about approaches to intervention and specific case management also occurred throughout the process.
As the project progressed a decision was made to develop a program rationale and prescription manual for orthotic intervention which was congruent with the model of Occupational Performance (Chapparo & Ranka, 1992). It was decided that this would address the thematic concern identified and was consistent with developments taking place in the Occupational Therapy Service of the Centre (Colyer, 1994). Continual reflection on the process and outcomes occurred throughout the project to ensure that decisions made were congruent with the views of the occupational therapists, the philosophy of the spinal unit and the larger Occupational Therapy Service of the Centre.
The outcome was a Policy and Procedure Manual for Upper Limb Orthotic Intervention in Occupational Therapy (Ranka, Colyer, Dickson & Chow, 1994) which contains:
- statement of beliefs and values
- theoretical framework
- program aims
- specific aims of orthotic intervention for each level of spinal injury
- assessment strategies
- orthotic patterns and fabrication guidelines
- program protocol
- methods to evaluate program effectiveness.
Readers interested in finding out more about the content of this manual are encouraged to contact the Service or the author directly. The remainder of this paper contains an extension and reconfiguration of aspects of this original work. It includes an example of a ‘beliefs and values’ statement, a theoretical rationale, program aims and an example of how they have been used to guide specific upper limb orthotic prescription in occupational therapy for clients whose hand function has been compromised by spinal cord injury.
OCCUPATIONAL PERFORMANCE: A PROGRAM GUIDE FOR THE PRESCRIPTION OF UPPER LIMB ORTHOTICS.
A statement of beliefs, values and assumptions.
The underlying beliefs, values and assumptions of the Occupational Performance Model (Australia) (Chapparo & Ranka, 1996) provide a vehicle for discussing these issues as they relate to the provision of orthotic systems in occupational therapy. The following is an example of a ‘Beliefs, Values and Assumptions’ statement related to clients with spinal cord injury and orthotic intervention in occupational therapy. It is an extension of the original work of Ranka, Colyer, Dickson & Chow (1994).
Occupational therapists believe that clients with a spinal cord injury have a right to equal opportunity in returning to their needed or desired occupational roles within the constraints of their disability and environments. We recognise that paralysis, muscle imbalance, and sensory loss which directly result from spinal cord injury will interfere with a clients ability to perform the activities and tasks required by these roles. Upper limb orthotic intervention is a primary method of intervention used by occupational therapists to prevent problems associated with loss of sensory and motor innervation to the upper limb and to enhance occupational role, routine and task performance.
Occupational therapists view clients as the directors of their care who are capable of making informed choices, and strive to involve them in all aspects of their occupational therapy program. We recognise that spinal cord injury is often accompanied by prolonged periods of emotional distress which can affect both the client and their family’s ability to process and act on information provided. As a result, we understand that neither the client nor their family may be able to make informed choices about suggested interventions until later in the adjustment process. For this reason, we believe it is imperative that orthoses are provided as soon as possible after injury to ensure optimum wrist and hand position for performance of occupational tasks involving gestural communication, manipulating tools, transporting objects and operating environmental and transportation controls until the client and/or their family choose to continue or discontinue their use.
Occupational therapists believe in a minimalist approach to orthotic prescription for the wrist and hand. This involves prescribing an orthosis which accomplishes its aims but is as unobtrusive as possible. We view any equipment provided as an integral part of the client’s personal belongings and will exercise care during fabrication to make all orthoses asaesthetically appealing as possible. We will treat both the client and their equipment with respect.
THEORETICAL FRAMEWORK:
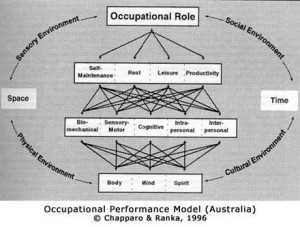
The theoretical foundation supporting upper limb orthotic prescription in occupational therapy is based on the Occupational Performance Model (Australia) (Chapparo & Ranka, 1996) (Fig. 1). Occupational performance is the ability to perceive, desire, recall, plan and perform roles, routines, tasks and subtasks for the purposes of self-maintenance, productivity/school, play/leisure and/or rest (Chapparo & Ranka, 1996) (Fig. 1).
Figure 1: Occupational Performance Model
Occupational performance results from the interactions occurring within and between the remaining seven constructs of the model, Occupational Performance Roles, Occupational Areas, Components of Occupational Performance, Core Elements, External Environment, Space and Time.
The use of this theoretical framework for upper limb orthotic prescription in occupational therapy ensures that occupational therapists consider more than deformity management and the enhancement of hand function in clients when making a clinical decision to prescribe an orthosis or not. Consideration of each construct in the model contributes to this decision.
Occupational Performance Roles
This interaction of constructs in this Model signify that the domain of concern of occupational therapy is the enhancement of occupational role performance. Occupational Performance Roles involve ‘doing’ the routines, tasks and sub-tasks required by a role, ‘knowing’ how these routines, tasks and sub-tasks are performed, and ‘being’ the type of performer one desires or is capable of. Upper limb orthotics are one technique used to enable people to ‘do’ what they choose to, ‘know’ how they can still perform in a role and ‘be’ in the roles they need or desire. For example, orthotic systems may be used to enable someone with a spinal cord injury to bring a fork to his mouth to eat (‘doing’) or members of a spinal cord injury cooking group may use their orthosis to prepare a meal (‘doing’). Another person with a spinal cord injury may use a tenodesis splint to learn how to transfer wrist extension muscle power into the prehension force required for transporting objects of various sizes and weights (‘knowing’). Alternatively, another person may not use her tenodesis orthosis but knows she can use it for specific tasks if she wants to (‘knowing’). Yet another person who is unable to move his upper limb may benefit from a positional orthosis which prevents deformity thereby allowing him to be a ‘son’ or ‘worker’ whose hand has a desired aesthetic appearance (‘being’).
Occupational Areas: Routines, Tasks & Subtasks:
Using the Occupational Performance Model (Australia), occupational therapists identify the roles a person wishes to return to or will be required to assume, and, then, identify with the client the tasks and routines required by these roles which are posing difficulty. These tasks and routines may include: self-maintenance tasks, productivity or school tasks, leisure or play tasks and rest tasks. Upper limb orthotics are prescribed specifically with these sub-tasks, tasks and routines in mind and orthotic-use training involves using the orthosis to practice methods of performing these tasks.
Components of Occupational Performance:
The routines, tasks and sub-tasks from these occupational areas require various human operations which, in this Model, are classified as biomechanical, sensory-motor, cognitive, intrapersonal and interpersonal. These component operations are a part of every sub-task, task, routine and occupational role. Some of the consequences of a spinal cord injury are reduced strength (biomechanical) and impaired differentiation between painful and non-painful stimuli (sensory-motor) which interfere with use of the limb. This, in turn, may also produce dysfunction in cognitive, intrapersonal and interpersonal operations. Upper limb orthotic systems are usually prescribed to maintain passive range of motion in the wrist and hand (biomechanical component), however, operations in the other component areas (cognitive component, intrapersonal component, interpersonal components) are also considered in order to optimise subtask, task, routine and occupational role performance.
Core Elements:
Underlying all of these Components of Occupational Performance is the body-mind-spirit unit. These ‘Core Elements’ are the human body, the human nervous system, the human mind, the human consciousness of self and the human awareness of the universe (Popper, 1981). They represent the fundamental uniqueness of each individual and experience the direct effects of a spinal cord injury. Upper limb orthotics may be prescribed to address the affect of disease processes, disorders and/or injuries to a client on these core elements as they influence that client’s total occupational performance. For example, a wrist-hand orthosis may be prescribed to promote soft tissue shortening at the metacarpal phalangeal joint into flexion (body). Another orthosis may be prescribed to demonstrate to a client that he is still worthy of care in spite of profound disability (mind, spirit).
External Environment:
As portrayed in the diagram of the Occupational Performance Model (Australia), the external environment has physical, sensory, social and cultural dimensions. The interaction of these aspects create political and economic subdivisions of the environment (Chapparo & Ranka, 1996). The environment constrains performance, can be modified by performance and may be an asset which supports performance. Upper limb orthotics are prescribed with consideration of all aspects of the environment. For example, a hot sensory environment may influence the choice of materials used in fabrication and client acceptance of the orthosis, or an orthosis may enable a client to control the environment more effectively as in managing electric wheelchair controls or operating a computer to access the internet. Political and economic factors may affect the options available.
Time and Space:
The presence of these two constructs in the Model signify that all transactions occurring between the constructs during occupational performance take place in both objective dimensions and personal interpretations of space and time. Occupational therapists consider the timing and duration of upper limb orthotic intervention and the ultimate form a client’s hand will take.
Summary of Implications for Practice:
Principles underlying the Occupational Performance Model (Australia) emphasise that the primary goal of occupational therapy is to enable persons or groups to identify, choose and perform needed or desired occupational roles including routines, activities, tasks and sub-tasks to the satisfaction of one’s self or significant others. Methods employed focus on this primary goal and consist of strategies to modify or compensate for dysfunctional aspects of the internal or external environment. The prescription, fabrication and provision of upper limb orthotic systems is one skill an occupational therapist may use to accomplish this broad aim.
POPULATION:
Ranka & Chapparo (1993) have stated that occupational therapists who use the Occupational Performance Model (Chapparo & Ranka, 1992, 1996) to guide practice address the occupational needs of their clients and that therapy provided which does not address this need, is not occupational therapy. Therefore, the prescription of upper limb orthotic systems will be considered for any client whose hand function has been compromised by spinal cord injury. A decision to prescribe an orthosis will be based on whether or not a client ‘occupational need’ is identified.
PROGRAM AIMS:
The aims of a program provide an indication of the focus of the program and the expected changes in client performance as a result of participation in the program. Consistent with the view described in the Occupational Performance Model (Australia) (Chapparo & Ranka, 1996), the broad aims of upper limb orthotic intervention include:
| Occupational Performance Roles: | |
| 1. | To provide clients with opportunities to achieve optimum occupational role performance; including ‘doing’, ‘knowing’ and ‘being’ dimensions. |
| Occupational Performance Areas: | |
| 2. | To enhance a client’s performance of routines, tasks and sub-tasks required by their roles in the areas of self-maintenance, leisure/play, productivity/ school and rest. |
| Other Dimensions of Occupational Performance: | |
| 3. | To address obstacles to role, routine, task or sub-task performance which arise from other areas identified in the Model. Aims which address these obstacles include: |
| Biomechanical Component Aims: | |
|
|
| Sensorymotor Aims: | |
|
|
| Cognitive Aims: | |
|
|
| Intrapersonal Aims: | |
|
|
| Interpersonal Aims: | |
|
|
| Core elements of Body-Mind-Spirit: | |
|
|
| Environment: | |
|
|
| Time & Space: | |
|
|
PRESCRIPTION GUIDELINES FOR LEVELS OF SPINAL CORD INJURY:
Guidelines for orthotic prescription which are consistent with the Occupational Performance Model (Australia) (Chapparo & Ranka, 1996) were developed by Ranka, Colyer, Dickson and Chow (1994) using orthotic protocols described by Chapparo (1980), Hill and Presperin (1986), Mallick and Meyer (1978) and personal experience. These have been developed further in this paper and are presented to illustrate how the constructs and principles of the Occupational Performance Model (Australia) (Chapparo & Ranka, 1996) can be used to develop a specific rationale for orthotic prescription.
At this time, these guidelines are limited to wrist-hand orthoses (WHO), hand orthoses (HO) and thumb orthoses (TO). An expanded version of this paper will include prescription principles for balanced forearm orthoses (BFO’s).
Procedures for client assessment, therapy regimes which incorporate the use of upper limb orthotics into a clients occupational performance and methods to evaluate the effectiveness of the program are also beyond the scope of this paper.
OCCUPATIONAL THERAPY PRESCRIPTION GUIDELINES FOR WRIST-HAND AND HAND ORTHOSES IN CLIENTS WITH SPINAL CORD INJURY
| C1-3 | Absent arm placement |
| 0 Wrist Musculature | |
| 0 Finger or Finger Musculature |
OCCUPATIONAL PERFORMANCE RATIONALE:
| 1. | To maintain a hand position which supports ‘knowing’ & ‘being’ aspects of occupational role performance. | ||||||||||||||||||||||||||||||||||||
| 2. | To enhance participation in routines, tasks and sub-tasks required by client occupational roles. | ||||||||||||||||||||||||||||||||||||
| 3. | To address other obstacles to occupational performance, including: | ||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||
| DAY POSITIONING: |
|
|||||||||||||||||||
| NIGHT POSITIONING: |
|
|||||||||||||||||||
| C4-5 | Limited arm placement |
| 0 Wrist Musculature | |
| 0 Finger or Thumb Musculature |
OCCUPATIONAL PERFORMANCE RATIONALE:
| 1. | To maintain a hand position which supports ‘doing’, ‘knowing’ & ‘being’ aspects of occupational role performance. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2. | To enhance performance of routines, tasks and sub-tasks required by client occupational roles. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3. | To address other obstacles to occupational performance, including: | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| DAY POSITIONING: |
|
|||||||||||||||||||
| NIGHT POSITIONING: |
|
|||||||||||||||||||
| FUNCTIONAL ORTHOSES: |
|
|||||
| C5-6 | Limited but functional arm placement |
| 0-3 Wrist Musculature | |
| 0 Finger or Thumb Musculature |
OCCUPATIONAL PERFORMANCE RATIONALE:
| 1. | To maintain a hand position which supports ‘doing’, ‘knowing’ & ‘being’ aspects of occupational role performance. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2. | To enhance performance of routines, tasks and sub-tasks required by client occupational roles. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3. | To address other obstacles to occupational performance, including: | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| DAY POSITIONING: |
|
|||||||||||||||||||||
| NIGHT POSITIONING: |
|
|||||||||||||||||||
| FUNCTIONAL ORTHOSES: |
|
|||||
| C6 | Functional arm placement to face, side and back of neck and partially across midline |
| 3+ to 5 Wrist Extension | |
| 0 Wrist Flexion | |
| 0 Finger or Thumb Musculature |
OCCUPATIONAL PERFORMANCE RATIONALE:
| 1. | To maintain a hand position which supports ‘doing’, ‘knowing’ & ‘being’ aspects of occupational role performance. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2. | To enhance performance of routines, tasks and sub-tasks required by client occupational roles. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3. | To address other obstacles to occupational performance, including: | ||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||
| DAY POSITIONING: |
|
|||||||||||||||||||
| NIGHT POSITIONING: |
|
|||||||||||||||||||||||||
| FUNCTIONAL ORTHOSES: |
|
|||||
| C7 | Full arm placement |
| 3+ to 5 Wrist Extension and Flexion | |
| 0-3 Extrinsic finger and thumb musculature | |
| 0 intrinsic finger thumb musculature |
OCCUPATIONAL PERFORMANCE RATIONALE:
| 1. | To maintain a hand position which supports ‘doing’, ‘knowing’ & ‘being’ aspects of occupational role performance. | ||||||||||||||||||||||||||||||||||||||||||
| 2. | To enhance performance of routines, tasks and sub-tasks required by client occupational roles. | ||||||||||||||||||||||||||||||||||||||||||
| 3. | To address other obstacles to occupational performance, including: | ||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||
| DAY POSITIONING: |
|
|||||||||||||||||||
| NIGHT POSITIONING: |
|
|||||||||||||||||||||||||
| FUNCTIONAL ORTHOSES: |
|
|||||||
| C8-T1 | Full arm placement and wrist function isolated finger and thumb weakness |
OCCUPATIONAL PERFORMANCE RATIONALE:
| 1. | To maintain a hand position which supports ‘doing’, ‘knowing’ & ‘being’ aspects of occupational role performance. | ||||||||||||||||||||||||||||||||||||||||||
| 2. | To enhance performance of routines, tasks and sub-tasks required by client occupational roles. | ||||||||||||||||||||||||||||||||||||||||||
| 3. | To address other obstacles to occupational performance, including: | ||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||
| DAY POSITIONING: | None except to manage specific problems resulting from weakness, muscle imbalance, spasm, etc. |
| NIGHT POSITIONING: | None, except to manage specific problems resulting from weakness, muscle imbalance, spasm, etc. |
SUMMARY:
The Occupational Performance Model (Australia) (Chapparo & Ranka, 1996) has been applied to the development of upper limb orthotic prescription guidelines for occupational therapists working in the area of spinal cord injuries. Using this Model, occupational therapists are directed to consider aspects of human function which go beyond deformity control and hand function when making clinical decisions in this area. Intervention focuses on using upper limb orthotics to address the occupational needs of clients by enhancing their occupational role performance.
Occupational therapists can use the prescription guideline presented here to construct their own program or to design occupation-centred research in this area of practice. For example, Ranka and Chapparo (1993) and Chapparo and Ranka (1996) suggest that the relationship between each construct in the model can be a question for research. The aims of intervention described in this paper reflect a relationships between constructs in the model. When these are posed as research questions, occupational therapists may investigate, for example:
Does specific orthotic intervention have an effect on gestural communication?
Does specific orthotic intervention have an effect on reach patterns required for specific occupational tasks?
Does specific orthotic intervention have an effect on speed and control of prehension patterns during performance of specific occupational tasks?
Does specific orthotic intervention have an effect on client perceptions of self-worth?
Does specific orthotic intervention have an effect on speed and accuracy of handwriting?
Answers to questions such as these will build a body of knowledge on which occupational therapists can make sound clinical decisions in this area of practice.
ACKNOWLEDGMENT:
The Occupational Therapy Service of the Royal Rehabilitation Centre Sydney and Moorong Spinal Unit.
REFERENCES:
Akeson, W.H. Amiel, D., Abel, M.R., Garfin, S.R., & Woo, S. L-Y. (1987). Effects of immobilisation on joints. Clinical Orthopedics and Related Research, 219, 28-37.
Anderson, M. (1965). Functional bracing of the upper extremities. Springfield, IL: Charles C. Thomas
Booth, F.W. (1987). Physiologic and biochemical effects of immobilisation on muscle. Clinical Orthopedics and Related Research, 219, 15-20
Boss, B.J. (1994). The neurophysiological basis of learning: concept formation/abstraction, reasoning and executinve functions — implications for SCI nurses (Part 2). SCI Nursing, 11(Mar), 3-6.
Botte, M.J., Nickel, V.L., & Akeson, W.H. (1988). Spasticity and contracture: Physiologic aspects of formation. Clinical Orthopedics, 8, 7-18.
Brand, P. (1985). Clinical mechanics of the hand. St. Louis: CV Mosby
Chapparo, C. (1980). Upper extremity orthotic systems for patients with quadriplegia. (Slide/sound training package). Chicago: RIC Education and Training Centre.
Chapparo, C., & Ranka, J. (1992). Occupational Performance, Draft Manuscript. (Available from authors, School of Occupational Therapy, The University of Sydney, PO Box 170, Lidcombe, NSW, Australia 2141)
Chapparo, C., & Ranka, J. (1996). Occupational Performance Model (Australia) Draft Manuscript. (Available from authors, School of Occupational Therapy, The University of Sydney, PO Box 170, Lidcombe, NSW, Australia 2141)
DiPasquale-Lehnertz, P. (1994). Orthotic intervention for development of hand function with C-6 quadriplegia. Amercian Journal of Occupational Therapy, 48(2), 138-144.
Guilford, A., & Perry, J. (1975). Orthotic components. In American Academy of Orthopedic Surgeons, Atlas of Orthotics: Biomechanical principles and application (pp. 81-104). St. Louis: CV Mosby
Hill, J. , & Presperin, J. (1986). Deformity control. In J. Hill (Ed.), Spinal cord injury: a guide to functional outcomes in occupational therapy (pp. 49-86). Rockville, MD: Aspen
Knox, C.C., Engel, W.H., & Siebens, A.A. (1971). Results of a survey on the use of a wrist-driven splint for prehension. American Journal of Occupational Therapy, 25, 109-111.
Lee, A.C. (1988). Survey of Rancho flexor hinge splint users. British Journal of Occupational Therapy, 51(6), 197-198.
Lightbody, S. (1994). Dynamic pronation splint in high level spinal cord injury: a case study. Australian Occupational Therapy Journal, 41(2), 83-85.
Lohman, M. (1982). Survey: current orthotic practices in occupational therapy. Orthotics and Prosthetics, 36(2), 42-48.
Mallick, M. (1965). Manual on static hand splinting: new materials and techniques. Pittsburgh, PA: Harmarville Rehabilitation Centre
Mallick, M., & Meyer, C. (1978). Manual on managementof the quadriplegic upper extremity. Pittsburg: Harmarville, Rehabilitation Centre.
Martin, C. (1987). Functional hand orthoses for quadriplegics: Long term use: 1987 American Spinal Injury Association Abstracts Digest, 372.
Newsom, M.J., Keenan, G., Maddry, J., & Aguilar, S. (1969). An occupational therapy training program for the C5-6 quadriplegic. American Journal of Occupational Therapy, 22, 126-129.
Nichols, P.J.R., Peach, S.L, Haworth, R.J., & Ennis, J. (1978). The value of hand splints. Prosthetic Orthotics, 2, 86-94.
Partridge, C. (1994). Spinal cord injuries: aspects of psychological care. British Journal of Nursing, 3(1), 12-15.
Patterson, D.R. (1993). Psychological intervention with spinal cord injured patients: promoting control out of dependence. SCI Psychosocial Process, 6(2), 2-8.
Perry, J. (1975b). Pathomechanics. In American Academy of Orthopedic Surgeons, Atlas of Orthotics: Biomechanical principles and application (pp. 57-64). St. Louis: CV Mosby
Popper, C. (1981). Part 1, In K. Popper, & J. Eccles, The self and its brain: an argument for interactionism (pp. 3-211). Berlin: Springer International
Ranka, J., & Chapparo, C. (1993, September). Occupational performance: A practice model for occupational therapy. Paper presented at the 6th State conference of OT Australia AAOT-NSW, Mudgee, NSW.
Ranka, J., Colyer, S., Dickson, K., & Chow, M. (1994). Orthotic prescription in occupational therapy at Moorong Spinal Unit. (Available from Occupational Therapy Department, Moorong Spinal Unit, Royal Rehabilitation Centre Sydney, Morrison Rd., Ryde, NSW)
Ranka, J., & Zhuo Dahong. (1987). Occupational therapy: a ten-day course for doctors. Course presented at Sun Yat-Sen University of Medical Sciences, Guangzhou, PRC
Sargant, C., & Braun, M.A. (1986). Occupational therapy management of the acute spinal cord-injured patient. American Journal of Occupatiional Therapy, 40, 333-337
Shepherd, C., & Ruzicka, S.H. (1991). Tenodesis brace use by persons with spinal cord injuries. American Journal of Occupational Therapy, 45(1), 81-83.
Sutton, S. (1993). An overview of the management of the C6 quadriplegic patient’s hand: an occupational therapist’s perspective. British Journal of Occupational Therapy, 56(10), 376-380..
Trombley, C. (1989). Orthoses: purposes and types. In C.A. Trombley (Ed.) Occupational therapy for physical dysfunction (pp. 329-355). Baltimore: Williams & Wilkins
Wilson, McKenzie, Barber, & Watson (1974). Spinal cord injury: A treatment guide for occupational therapists (2nd ed.). Thorofare, NJ: Slack, Inc.
Wilson, McKenzie, Barber, & Watson (1984). Spinal cord injury: A treatment guide for occupational therapists (2nd ed.). Thorofare, NJ: Slack, Inc.
Wise, M., Wharton, g., & Robinson, T. (1980). Long term use of functional hand orthoses by quadriplegics. 1980 American Spinal Injury Association Abstracts Digest, 45.
Wynn Parry, C.B., Berkeley, C. (1981). Rehabilitation of the hand (4th ed.). London: Butterworth
Yarkony, G. (1990). A new orthosis for central cord syndrome and brachial plexus injuries. Archives of Physical Medicine & Rehabilitation, 71(12), 1006-1009.
Yarkony, G., Bass, M., Keenan, B., & Meyer, P. (1985). Contractures complicating spinal cord injury: Incidence and comparison between spinal cord centre and general hospital acute care. Paraplegia 23, 265-271.